Manifestations and diagnosis of the disease
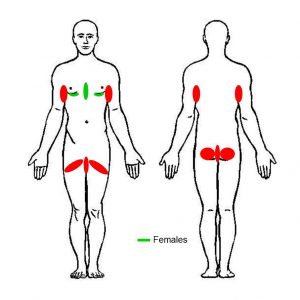
HS presents a variable clinical course. One of the main features of the disease is the intertriginous occurrence, although other areas of skin may also be affected. The affected areas in decreasing order of frequency are: inguinal, axillary, perineal and perianal, as well as the submammary and/or intermammary fold in women, buttocks, mons pubis, scalp, behind the ears and eyelids (Fig. 1).
The initial transient superficial lesions, namely follicular papules and pustules (folliculitis) are not diagnostic.
Important Note!
- Diagnosis of HS requires examining all body areas in which the disease can occur by the naked eye and without clothes.
- It is not appropriate to just ask the patients about skin lesions in these areas.
Primary care setting
Outbreaks of boils during the last 6 months with a minimum of two boils with five different location options [axilla, groin, genitals, under the breasts and other locations (not specified), e.g. perianal, neck and abdomen]
Dermatology clinics setting
Obligatory criteria
- History: Recurrent painful or purulent lesions more than 2x/6 months
- Location: groin, armpit, perineum, buttocks area and submammary/intramammary fold (women)
- Clinical signs:
- Primary lesions: Follicular papule/pustule (folliculitis), nodule (inflammatory or non-inflammatory), abscess
- Secondary lesions: Cyst, fistula/sinus (exudative or non-exudative), double pseudocomedone, scar (atrophic, net-like, erythematous, hypertrophic, linear or bridged)
Additional criteria (not obligatory)
- History: HS-positive family history
- Microbiology: No evidence of pathogens or presence of normal skin microflora at the predominant primary type of lesions
Diagnosis of HS if
- all three criteria are present
- one or more obligatory locations are involved
- one or more types of obligatory lesions are present (lesions in bold letters are obligatory lesions)
Transient or persisting inflammatory nodules, abscesses and draining tunnels (fistules and sinuses) are part of the diagnostic definition, leading to scars than can gradually coalesce to form plaques (Fig. 2). 23-30% of HS patients are also affected by a pilonidal sinus disease.
Fig. 2
Clinical manifestations: (a) Follicular papules/pustules (folliculitis), (b) nodules (left, non-inflammatory; right, inflammatory), (c) abscesses, (d) upper left, cysts in scar tissue; upper right and lower left, fistulae; lower right, sinuses, (e) left, double pseudocomedone and scars; right, scars
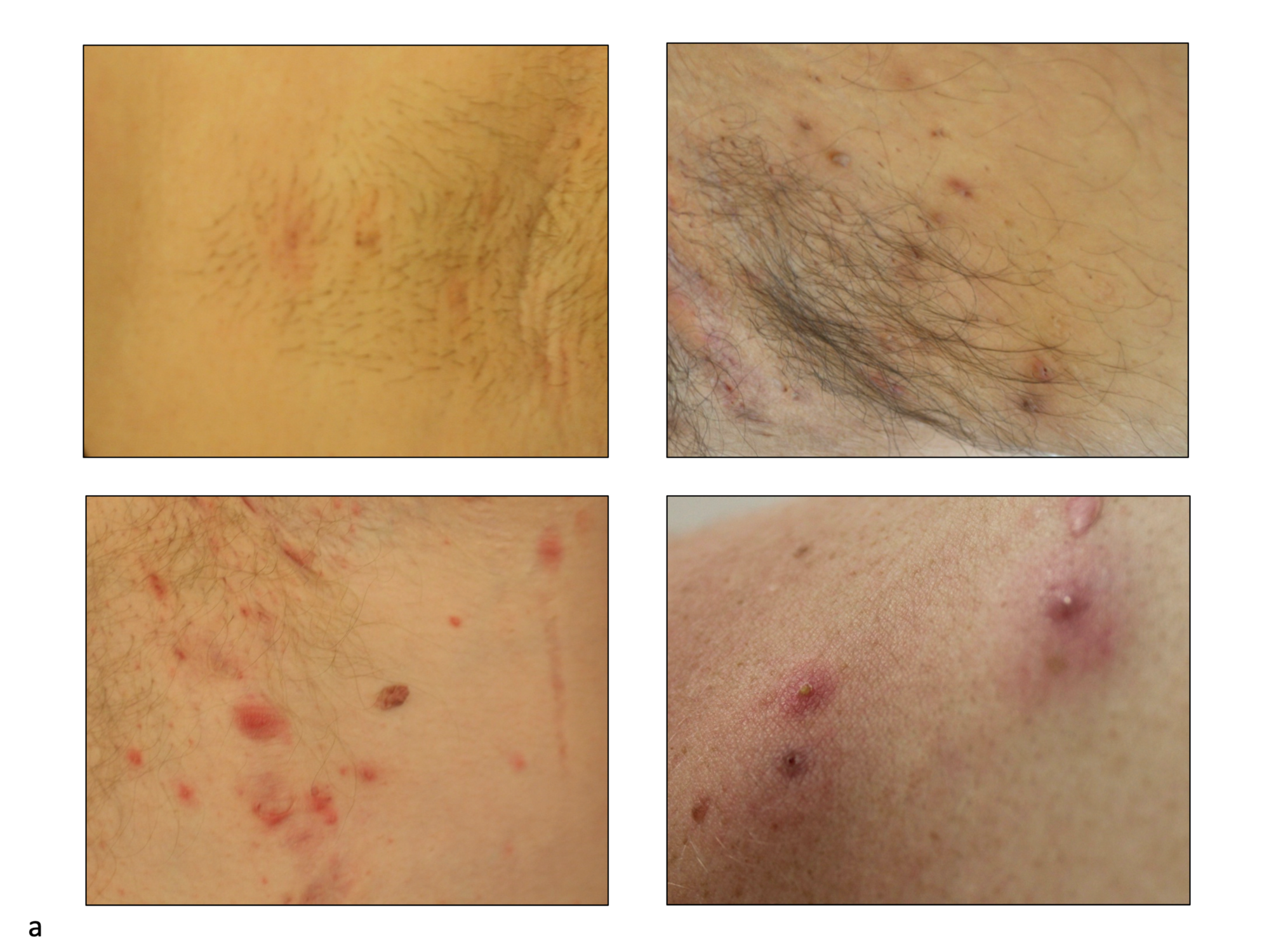
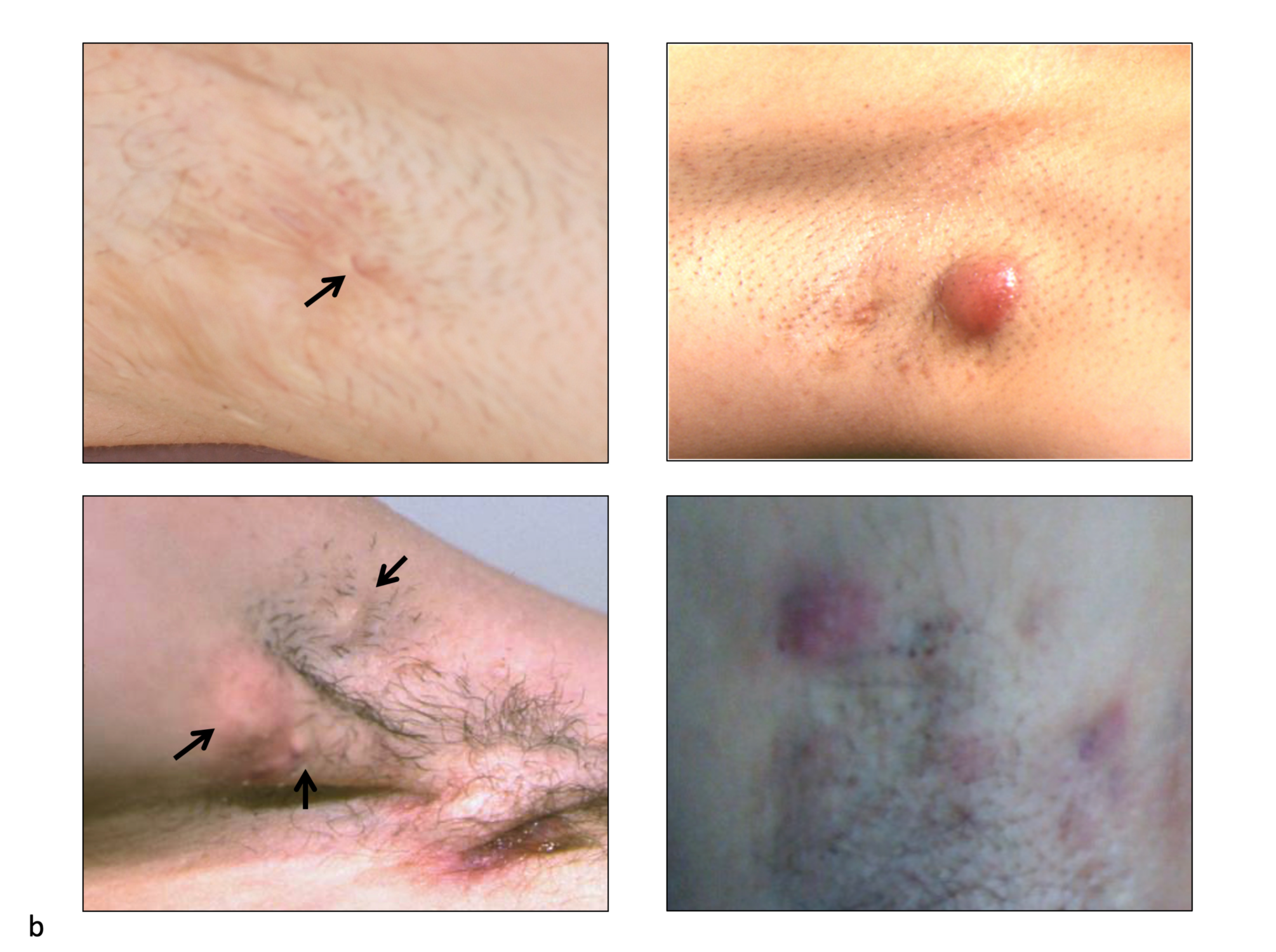
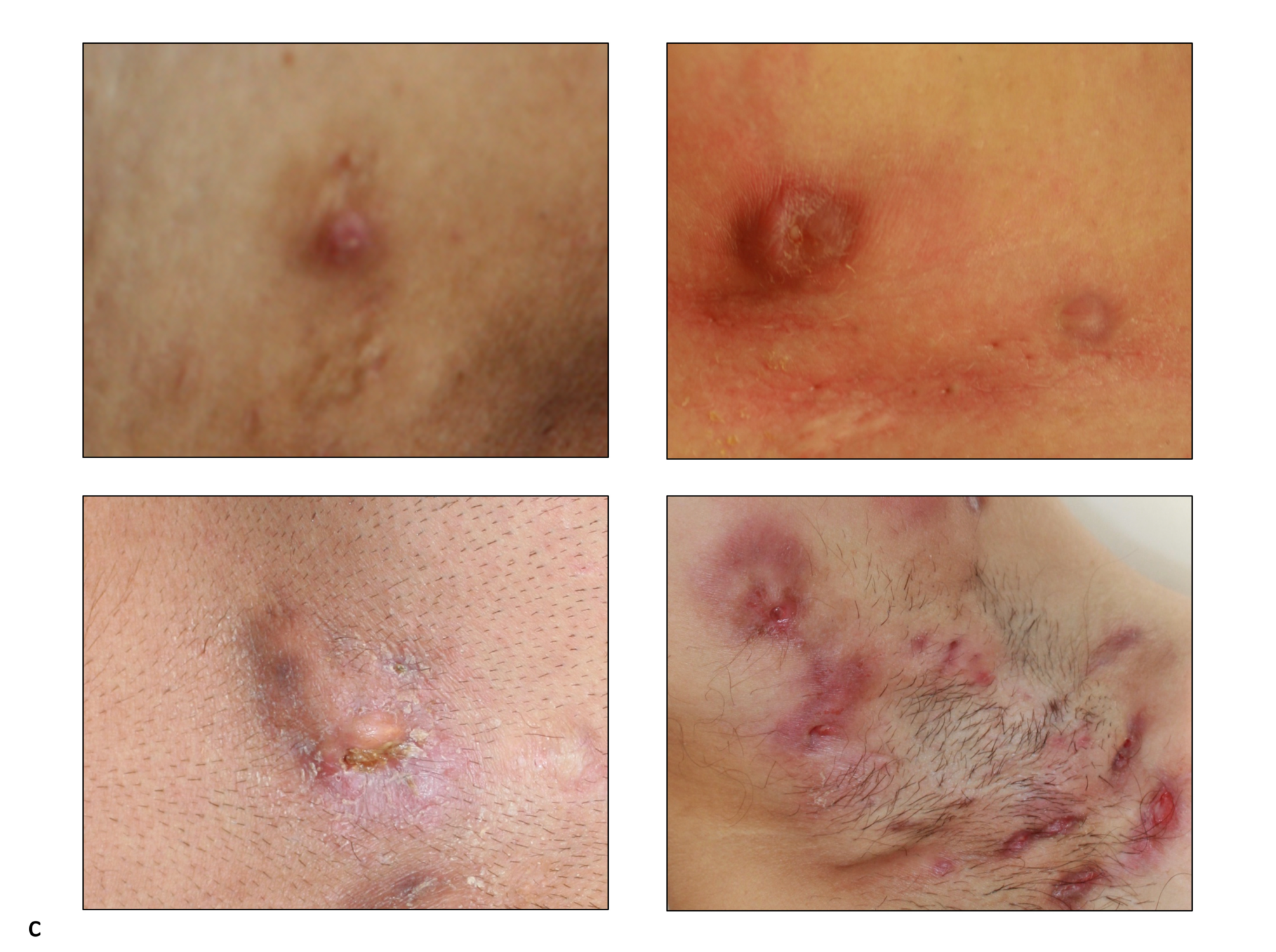
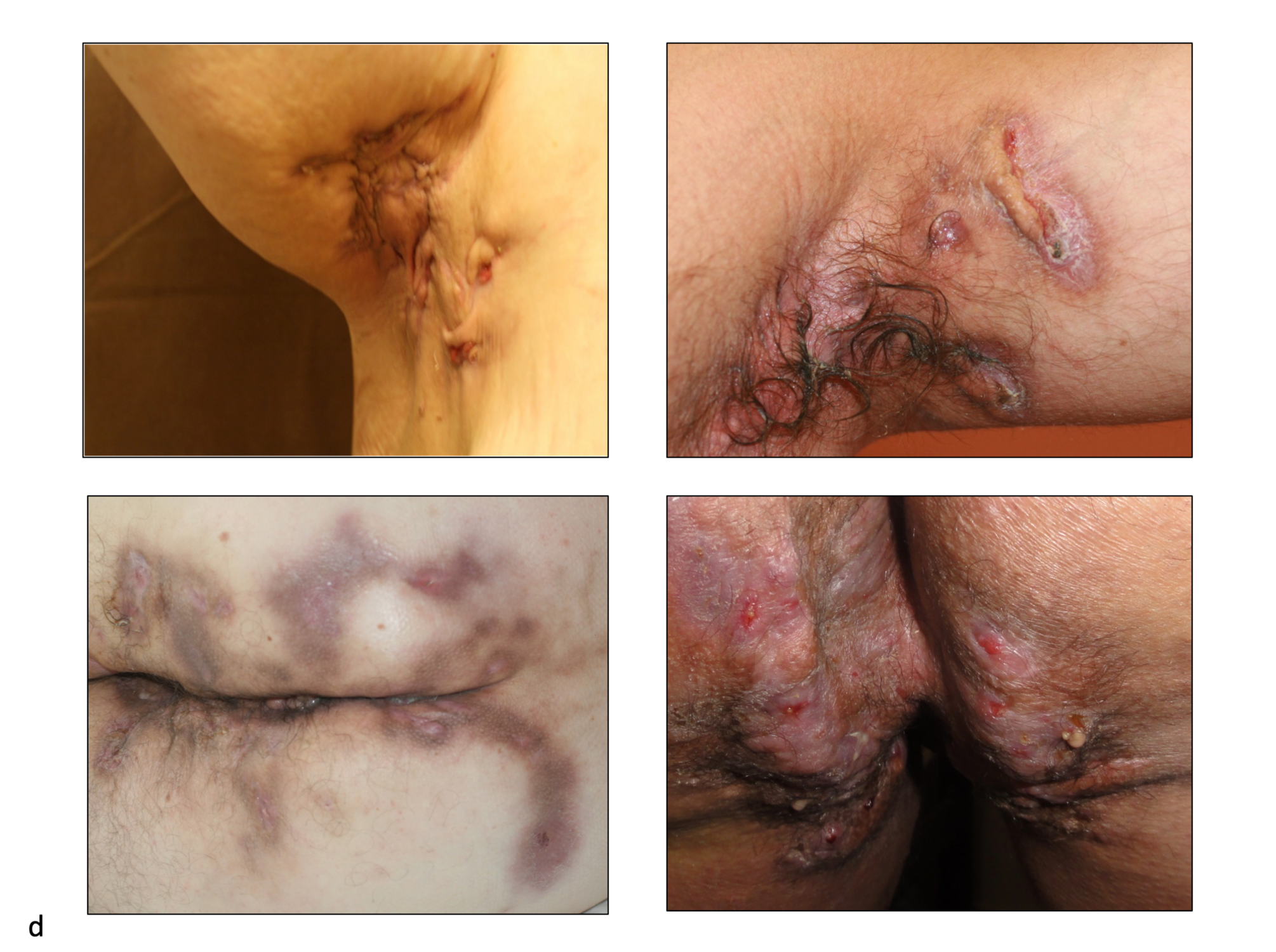

(From: Zouboulis CC, del Marmol V, Mrowietz U, Prens E, Tzellos T, Jemec GBE (2015) Hidradenitis suppurativa/acne inversa: Criteria for diagnosis, severity assessment, classification and disease evaluation. Dermatology 231:184-190, 2015)
